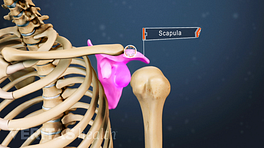
People typically recognize a shoulder dislocation right away, because it often occurs suddenly as the result of trauma during which the person experiences a “popping” sensation followed by shoulder pain and/or inability to move the arm.
Posterior shoulder dislocations are commonly misdiagnosed.
Most dislocations are anterior dislocations—in which the humeral head moves out of the socket to the front of the body—and their diagnosis is fairly straightforward. However, a rarer type of dislocation is frequently overlooked by physicians. Posterior (back of body) dislocations account for only 2 to 4% of shoulder dislocation, 1 Dumont GD, Russell RD, Robertson WJ. Anterior shoulder instability: a review of pathoanatomy, diagnosis and treatment. Curr Rev Musculoskelet Med. 2011;4(4):200-7 but may be initially misdiagnosed up to 60% of the time. 2 Hatzis N, Kaar TK, Wirth MA, Rockwood CA. The often overlooked posterior dislocation of the shoulder. Tex Med. 2001;97(11):62-7.
Diagnosing a shoulder dislocation normally involves a thorough medical history and physical examination. Imaging tests may also be taken to confirm a diagnosis.
In This Article:
Medical History
During the medical history portion of the exam, the physician will ask the patient questions about the following:
- The incident that caused the injury
- Symptoms, and how they impact activities
- Medical history and history of any shoulder injuries or treatment
If the dislocation has already been reduced (moved back into the socket), the physician may also want to know if this occurred spontaneously or with the help of someone else.
Physical Evaluation
The physical evaluation for a dislocated shoulder typically consists of palpation (touching) and observation, as well as range of motion and strength tests.
- Palpation and observation. The physician touches the injured shoulder, noting areas of tenderness and observing abnormalities. For example, there may be a bump visible at the front of the shoulder.
- Range of motion and strength tests. There are many physical tests a physician may use to help diagnose a shoulder dislocation. During these tests, the physician may note a person’s range of motion and degree of shoulder rotation.
Based on the physical examination, the physician will be able to make a diagnosis or will order medical imaging to get more information.
Imaging Tests
If the physician wishes to perform an imaging test to confirm the diagnosis, an x-ray is nearly always sufficient. Occasionally an MRI, MRI arthrogram (using contrast dye), or CT scan may be used to identify damage to nearby tendons, ligaments, or other soft tissues.
Treatment for a dislocated shoulder begins with reduction (resetting the shoulder joint), followed by immobilization in a sling. Most dislocations are initially treated with nonsurgical methods, which may lead to surgery if shoulder instability persists.