Featured Health Topics
5 Best Stretches and Exercises for Hip Labral Tears
Relieve hip labral tear pain quickly and effectively by stretching and strengthening the muscles in the lower back, buttock, pelvis, hip, and thigh.
Jumper’s Knee vs. Runner’s Knee
3 Simple Stretches for Hip Pain Relief
Relieve pain deep in your hip joint, around your hip area, and in your hip and thigh with these 3 targeted exercises.
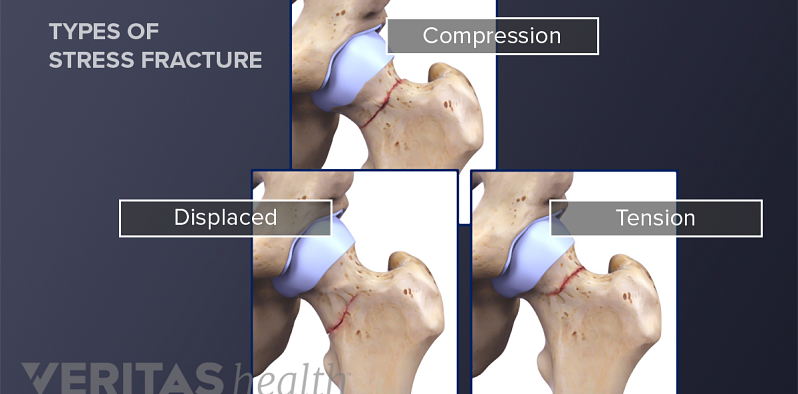
All About Stress Fractures
Spotlight on your health
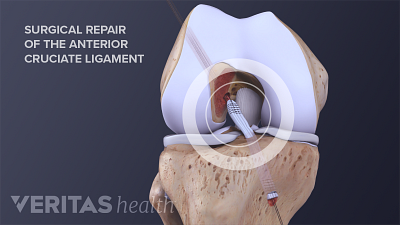
ACL Tear Surgical Repair
ACL tear surgical repair involves reconstructing the torn ligament using grafts, promoting knee stability and function postoperatively.
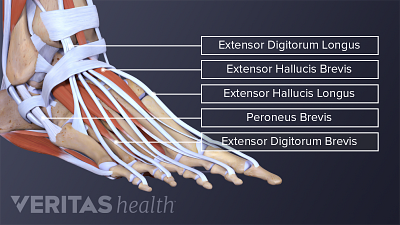
All About Ankle Sprains and Strains
Learn about ankle sprains and strains, common injuries involving ligaments or muscles, and their causes, symptoms, and treatment options.
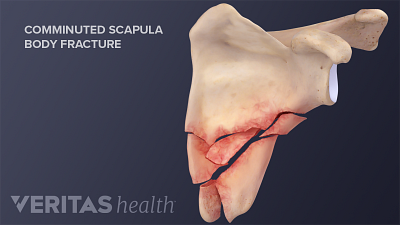
A Broken Shoulder: Scapula Fracture
Scapula fractures occur in the shoulder bone and cause severe pain, bruising, and weakness in the shoulder.
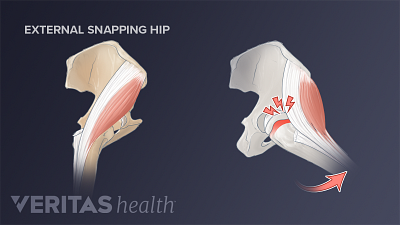
3 Types of Snapping Hip Syndrome
Internal, external, and intra-articular are the three types of Snapping Hip Syndrome, each involving distinct mechanisms of hip joint snapping.
Editors Top Picks
Both osteoarthritis and torn meniscus cause knee pain and restricted mobility but exhibit differences in patterns of onset, sensation, and recurrence of pain.
Listening to your body and being proactive about addressing even the smallest signs of shoulder pain can help to prevent further shoulder damage down the road.
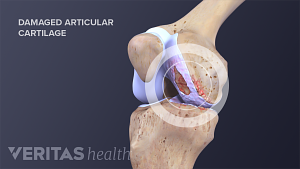
Damaged cartilage cannot grow back, so treating it necessitates regenerative treatments or surgery to facilitate regrowth and restoration of the cartilage.