The surfaces of bones that contact each other in a joint are coated with articular cartilage—a smooth tissue that provides a slippery surface for the bones to glide against each other in a frictionless manner.1Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009;1(6):461-468. doi:10.1177/1941738109350438
In This Blog:
Can cartilage grow back?
When damaged, the cartilage in the joints has a limited capacity to grow back or heal, making interventions to repair or regrow the cartilage necessary.1Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009;1(6):461-468. doi:10.1177/1941738109350438
Articular or joint cartilage is also called hyaline cartilage and is one of the five distinct types of cartilage.
How damaged cartilage feels
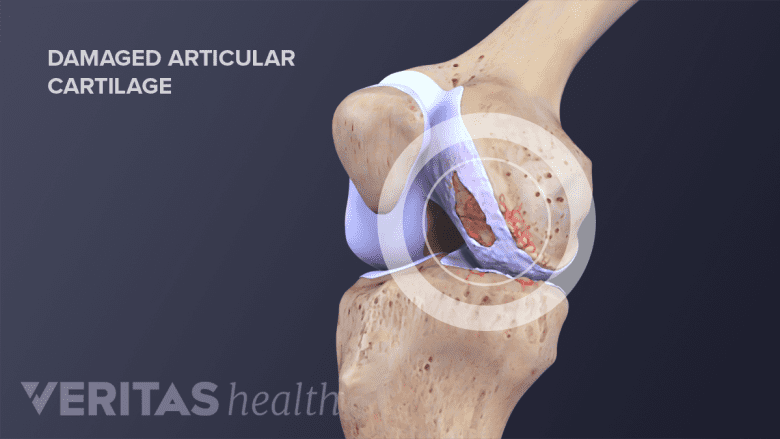
When articular cartilage is damaged, it cannot heal or regrow on its own.
Damage to the articular cartilage can occur due to traumatic injuries or repetitive strain. Such damage is often linked to a sevenfold heightened likelihood of developing osteoarthritis.2Liu Y, Shah KM, Luo J. Strategies for Articular Cartilage Repair and Regeneration. Front Bioeng Biotechnol. 2021 Dec 17;9:770655. doi: 10.3389/fbioe.2021.770655.
The signs and symptoms of acute articular cartilage damage include3Żylińska B, Sobczyńska-Rak A, Lisiecka U, Stodolak-Zych E, Jarosz Ł, Szponder T. Structure and Pathologies of Articular Cartilage. In Vivo. 2021;35(3):1355-1363. doi:10.21873/invivo.12388:
- Swelling and pain in the affected joint
- Cracking or grinding sounds during joint movement (crepitus)
- Limited range of motion
Over time, these symptoms and signs can potentially worsen as the joint's surfaces undergo further cartilage deterioration.
Joints prone to articular cartilage problems
Damage to the articular cartilage is common in the knee, shoulder, and hip joints. Damage may involve small lesions in the articular cartilage on one of the bones or complete loss of cartilage on both bones that articulate at the joint.
Regenerative treatments to repair damaged cartilage
Regenerative medicine aims to regrow cartilage in the affected joint. In regenerative medicine, cells or 3D-cell cultures are introduced into the joint space to help stimulate the regeneration of cartilaginous tissue at the site of damage.
Autologous chondrocyte implantation
Autologous chondrocyte implantation aims to regenerate injured cartilage by stimulating healing with chondrocyte cells.4Makris EA, Gomoll AH, Malizos KN, Hu JC, Athanasiou KA. Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol. 2015;11(1):21-34. doi:10.1038/nrrheum.2014.157
- A small portion of healthy joint tissue is surgically removed from a low-weight-bearing region of a donor joint, such as the knee joint, during the first surgery.5Andrade R, Vasta S, Pereira R, et al. Knee donor-site morbidity after mosaicplasty - a systematic review. J Exp Orthop. 2016;3(1):31. doi:10.1186/s40634-016-0066-0
- The chondrocyte cells in this healthy tissue are separated and cultured in the laboratory.
- The cultured chondrocytes are then transplanted back to the injury site (such as the ankle or the hip) during a second surgical procedure and covered with a thin tissue membrane.
A study that tracked 771 patients with knee cartilage lesions over a span of 11 years revealed an 82% success rate following an autologous chondrocyte implantation procedure. The average age of the patients was 33 years, and the efficacy of autologous chondrocyte implantation declined with an increase in age and cartilage lesion size.6Pareek A, Carey JL, Reardon PJ, Peterson L, Stuart MJ, Krych AJ. Long-Term Outcomes after Autologous Chondrocyte Implantation: A Systematic Review at Mean Follow-Up of 11.4 Years. Cartilage. 2016;7(4):298-308. doi:10.1177/1947603516630786
Platelet-rich plasma

PRP uses the patient's blood to repair damaged tissues like cartilage, tendons, ligaments, and muscles.
Platelet-rich plasma therapy involves delivering a concentrated solution of platelets (type of cell present in the blood), white blood cells, and growth factors into the affected joint via an injection.7Saita Y, Kobayashi Y, Nishio H, et al. Predictors of Effectiveness of Platelet-Rich Plasma Therapy for Knee Osteoarthritis: A Retrospective Cohort Study. J Clin Med. 2021;10(19):4514. Published 2021 Sep 29. doi:10.3390/jcm10194514
See Platelet-Rich Plasma Injection Procedure
Platelets secrete growth factors that stimulate the proliferation and differentiation of chondrocytes to grow back articular cartilage.
A study consisting of 517 patients with knee osteoarthritis reported that platelet-rich plasma therapy was effective in reducing pain in around 62% of participants with cartilage damage from knee osteoarthritis.7Saita Y, Kobayashi Y, Nishio H, et al. Predictors of Effectiveness of Platelet-Rich Plasma Therapy for Knee Osteoarthritis: A Retrospective Cohort Study. J Clin Med. 2021;10(19):4514. Published 2021 Sep 29. doi:10.3390/jcm10194514
Read more: Are PRP Injections Effective?
Stem cell therapy
Mesenchymal stem cells present in the bone marrow proliferate and differentiate to form cells that generate bone, cartilage, and fat surrounding the skeletal tissue.2Liu Y, Shah KM, Luo J. Strategies for Articular Cartilage Repair and Regeneration. Front Bioeng Biotechnol. 2021 Dec 17;9:770655. doi: 10.3389/fbioe.2021.770655.
Mesenchymal stem cells delivered via surgical implantation or injection help regrow the articular cartilage by:
- Dividing and differentiating to form chondrocytes in the presence of specific growth factors and other biological molecules
- Secreting growth factors that promote the proliferation and differentiation of cells
- Secreting molecules that reduce inflammation
Besides the bone marrow, mesenchymal stem cells are also present in the adipose tissue (fat) and the bloodstream and can be easily harvested for articular cartilage regeneration.
A recent study involving 329 participants found that stem cell therapy to treat knee osteoarthritis led to a reduction of over 50% in pain levels. This reduction in pain was observed for a period of up to two years following the treatment.8Freitag J, Wickham J, Shah K, Tenen A. Real-world evidence of mesenchymal stem cell therapy in knee osteoarthritis: a large prospective two-year case series. Regen Med. 2022;17(6):355-373. doi:10.2217/rme-2022-0002
See Does Stem Cell Therapy Work?
However, because most studies examining the effectiveness and safety of mesenchymal stem cells have a follow-up period of only about 2 years, concerns remain about the long-term safety of stem cell therapy.
Read more about Stem Cell Therapy for Sports Injuries
Matrix autologous cartilage Implantation (MACI)
MACI is a newer treatment that involves harvesting chondrocyte cells and growing them on a collagen-based membrane. This membrane is then surgically implanted in the joint to encourage cartilage regeneration.
Surgical repair of damaged cartilage
The objective of surgical repair for early-stage articular cartilage damage is to either elicit a healing response from the bone tissue or replace it with healthy cartilage.1Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009;1(6):461-468. doi:10.1177/1941738109350438 Severe damage to the articular cartilage requires joint replacement surgery.
Microfracture
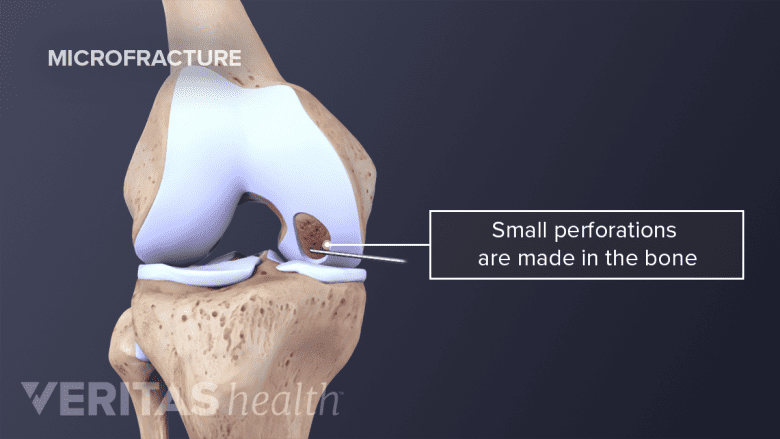
Microfracture helps by stimulating the growth of fibrocartilage to repair damaged joint surfaces.
Microfracture is a surgical technique that is used to repair small cartilage defects observed in young, active adults under the age of 40 years.
- Microfracture involves the removal of the damaged cartilage, followed by making several small perforations in the bony subchondral tissue that lies underneath the cartilage.
- These small perforations induce the mesenchymal stem cells in the bone to form fibrocartilage, a type of cartilage that is distinct from articular cartilage.
- Fibrocartilage is less flexible and less durable than hyaline cartilage.
The lower durability of fibrocartilage makes it susceptible to degeneration with time.
Drilling and subchondral abrasion
Drilling and abrasion arthroscopy are similar to microfracture and involve stimulating the bony tissue to produce fibrocartilage.
- Drilling involves the use of a surgical drill to make multiple holes and induce the healing response. Drilling is less precise than microfracture and has the potential to cause damage to healthy tissue due to heat.
- Subchondral abrasion involves the use of a bone drilling tool to provoke a healing response and, similar to drilling, is less precise than microfracture.
These procedures are typically used in younger adults with limited cartilage damage.
Osteochondral autograft transplantation: Transplanting the patient’s own bone
Osteochondral autografts involve the transplantation of hyaline cartilage and the underlying subchondral bone from non-weight-bearing regions of the same joint.9Branam GM, Saber AY. Osteochondral Autograft Transplantation. [Updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560655/ The grafts are harvested from single or multiple sites from the joint and transplanted in the damaged area during the same procedure.
For example, one or more small sections of cartilage and bone are taken from different regions of the knee. The graft is then transplanted in the center – where the damage is more prominent – to help regenerate cartilage tissue in that region.
Osteochondral allograft transplantation: Obtaining bone from a cadaver donor
Osteochondral allograft transplantation involves the surgical implantation of cartilage obtained from a cadaver donor, known as an allograft, at the affected site.
Total joint replacement
Severe damage to the articular cartilage that cannot be regenerated or stimulated is treated with partial or complete joint replacement surgery.2Liu Y, Shah KM, Luo J. Strategies for Articular Cartilage Repair and Regeneration. Front Bioeng Biotechnol. 2021 Dec 17;9:770655. doi: 10.3389/fbioe.2021.770655.
During joint replacement surgery, the defective cartilage is removed and replaced with a prosthetic made of metal, ceramic, or polymer.
Self-care to relieve discomfort associated with damaged cartilage
Self-care and at-home treatments can be useful in alleviating pain due to cartilage damage and preventing further degeneration but are not effective in reversing articular damage.
Medications
Over-the-counter pain relievers, such as ibuprofen and acetaminophen, help provide relief from pain and discomfort in the short term. Controlling inflammation with the help of oral non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroid injections is often necessary to engage in other treatments, such as physical therapy and exercise.
Resistance and aerobic exercise
Research indicates that engaging in resistance exercises or aerobic activities like walking, cycling, and swimming may lead to improvements in cartilage health among individuals with existing cartilage damage.10Hanaoka C, Fausett C, Jayabalan P. Nonsurgical Management of Cartilage Defects of the Knee: Who, When, Why, and How?. J Knee Surg. 2020;33(11):1078-1087. doi:10.1055/s-0040-1713813
A trained physical therapist can help develop a specific treatment plan that targets healing in the injured cartilage and joint.
Diet
A diet rich in monounsaturated fatty acids (MUFAs) and polyunsaturated fatty acids (PUFAs) has proven to reduce inflammation and potentially improve cartilage health. Omega-3 PUFAs are present in fish oil, walnuts, and flaxseed and are associated with lower inflammation and better cartilage health.11Cordingley DM, Cornish SM. Omega-3 Fatty Acids for the Management of Osteoarthritis: A Narrative Review. Nutrients. 2022;14(16):3362. Published 2022 Aug 16. doi:10.3390/nu14163362
A Mediterranean diet rich in fruits, vegetables, legumes, whole grains, beans, olive oil, and white meat is also associated with lower inflammation and improvements in joint health.12Veronese N, Koyanagi A, Stubbs B, et al. Mediterranean diet and knee osteoarthritis outcomes: A longitudinal cohort study. Clin Nutr. 2019;38(6):2735-2739. doi:10.1016/j.clnu.2018.11.032
Supplements
Supplements provide essential nutrients for joint health in concentrations that are difficult to achieve through typical dietary sources.
Over-the-counter supplements with established efficacy in enhancing cartilage well-being and promoting joint health comprise:
- Glucosamine and chondroitin sulfate. Glucosamine and chondroitin sulfate are components of healthy cartilage that help cushion the joint.
- Studies have generally used between 500-1500 mg each of chondroitin sulfate and glucosamine.13Simental-Mendía M, Sánchez-García A, Vilchez-Cavazos F, Acosta-Olivo CA, Peña-Martínez VM, Simental-Mendía LE. Effect of glucosamine and chondroitin sulfate in symptomatic knee osteoarthritis: a systematic review and meta-analysis of randomized placebo-controlled trials. Rheumatol Int. 2018;38(8):1413-1428. doi:10.1007/s00296-018-4077-2
- Curcumin. Evidence suggests that curcumin, the active ingredient present in turmeric, is effective in relieving pain.14Hsiao AF, Lien YC, Tzeng IS, Liu CT, Chou SH, Horng YS. The efficacy of high- and low-dose curcumin in knee osteoarthritis: A systematic review and meta-analysis. Complement Ther Med. 2021 Dec;63:102775. doi: 10.1016/j.ctim.2021.102775.
- A dose of around 500-1000 mg of curcumin supplement containing 95% curcuminoids is generally recommended for musculoskeletal conditions.
- Omega-3 supplements. Omega-3 supplements help reduce inflammation and prevent the degeneration of cartilage.15Cordingley DM, Cornish SM. Omega-3 Fatty Acids for the Management of Osteoarthritis: A Narrative Review. Nutrients. 2022;14(16):3362. Published 2022 Aug 16. doi:10.3390/nu14163362
- Omega-3 supplements include fish oil, algal oil, krill oil, and flaxseed oil.
It is important to note that these supplements are not regulated by the FDA. It is advisable to consult a physician to determine the appropriate dosage.
It is also important to talk with a physician or licensed dietician before trying a new diet, home remedy, or supplement to make sure it does not adversely interfere with underlying health conditions or current medications.
- 1 Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009;1(6):461-468. doi:10.1177/1941738109350438
- 2 Liu Y, Shah KM, Luo J. Strategies for Articular Cartilage Repair and Regeneration. Front Bioeng Biotechnol. 2021 Dec 17;9:770655. doi: 10.3389/fbioe.2021.770655.
- 3 Żylińska B, Sobczyńska-Rak A, Lisiecka U, Stodolak-Zych E, Jarosz Ł, Szponder T. Structure and Pathologies of Articular Cartilage. In Vivo. 2021;35(3):1355-1363. doi:10.21873/invivo.12388
- 4 Makris EA, Gomoll AH, Malizos KN, Hu JC, Athanasiou KA. Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol. 2015;11(1):21-34. doi:10.1038/nrrheum.2014.157
- 5 Andrade R, Vasta S, Pereira R, et al. Knee donor-site morbidity after mosaicplasty - a systematic review. J Exp Orthop. 2016;3(1):31. doi:10.1186/s40634-016-0066-0
- 6 Pareek A, Carey JL, Reardon PJ, Peterson L, Stuart MJ, Krych AJ. Long-Term Outcomes after Autologous Chondrocyte Implantation: A Systematic Review at Mean Follow-Up of 11.4 Years. Cartilage. 2016;7(4):298-308. doi:10.1177/1947603516630786
- 7 Saita Y, Kobayashi Y, Nishio H, et al. Predictors of Effectiveness of Platelet-Rich Plasma Therapy for Knee Osteoarthritis: A Retrospective Cohort Study. J Clin Med. 2021;10(19):4514. Published 2021 Sep 29. doi:10.3390/jcm10194514
- 8 Freitag J, Wickham J, Shah K, Tenen A. Real-world evidence of mesenchymal stem cell therapy in knee osteoarthritis: a large prospective two-year case series. Regen Med. 2022;17(6):355-373. doi:10.2217/rme-2022-0002
- 9 Branam GM, Saber AY. Osteochondral Autograft Transplantation. [Updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560655/
- 10 Hanaoka C, Fausett C, Jayabalan P. Nonsurgical Management of Cartilage Defects of the Knee: Who, When, Why, and How?. J Knee Surg. 2020;33(11):1078-1087. doi:10.1055/s-0040-1713813
- 11 Cordingley DM, Cornish SM. Omega-3 Fatty Acids for the Management of Osteoarthritis: A Narrative Review. Nutrients. 2022;14(16):3362. Published 2022 Aug 16. doi:10.3390/nu14163362
- 12 Veronese N, Koyanagi A, Stubbs B, et al. Mediterranean diet and knee osteoarthritis outcomes: A longitudinal cohort study. Clin Nutr. 2019;38(6):2735-2739. doi:10.1016/j.clnu.2018.11.032
- 13 Simental-Mendía M, Sánchez-García A, Vilchez-Cavazos F, Acosta-Olivo CA, Peña-Martínez VM, Simental-Mendía LE. Effect of glucosamine and chondroitin sulfate in symptomatic knee osteoarthritis: a systematic review and meta-analysis of randomized placebo-controlled trials. Rheumatol Int. 2018;38(8):1413-1428. doi:10.1007/s00296-018-4077-2
- 14 Hsiao AF, Lien YC, Tzeng IS, Liu CT, Chou SH, Horng YS. The efficacy of high- and low-dose curcumin in knee osteoarthritis: A systematic review and meta-analysis. Complement Ther Med. 2021 Dec;63:102775. doi: 10.1016/j.ctim.2021.102775.
- 15 Cordingley DM, Cornish SM. Omega-3 Fatty Acids for the Management of Osteoarthritis: A Narrative Review. Nutrients. 2022;14(16):3362. Published 2022 Aug 16. doi:10.3390/nu14163362

