Approximately 20% of people with chronic high (proximal) hamstring tendinopathy who undergo non-invasive (conservative) treatment, such as rest and physical therapy, have residual hamstring pain. 1 Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med 2009;37:727-34. , 2 Puranen J, Orava S. The hamstring syndrome--a new gluteal sciatica. Ann Chir Gynaecol 1991;80:212-4. , 3 Fredericson M, Moore W, Guillet M, Beaulieu C. High Hamstring Tendinopathy in Runners: Meeting the Challenges of Diagnosis, Treatment, and Rehabiliation. Phys Sports Med 2005;33:32-43. , 4 Zissen M, Wallace G, Stevens K, Fredericson M, Beaulieu C. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol 2010;195:993-8. , 5 Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med 2008;36:1110-5. For those that find no relief from non-invasive (conservative) management, minimally invasive treatments such as ultrasound-guided corticosteroid injections, ultrasound-guided needle tenotomy, ultrasound-guided platelet-rich plasma (PRP) injections, or ultrasound-guided percutaneous (through the skin) ultrasonic tenotomy may be pursued.
In This Article:
- Chronic High (Proximal) Hamstring Tendinopathy
- Symptoms of Chronic High (Proximal) Hamstring Tendinopathy
- High (Proximal) Hamstring Tendinopathy Risk Factors
- Diagnosing Chronic High (Proximal) Hamstring Tendinopathy
- Treatments for Chronic High Hamstring Tendinopathy
- Minimally Invasive Treatments for Chronic High Hamstring Tendinopathy
- Surgery for Chronic High (Proximal) Hamstring Tendinopathy
Steroid Injections
Injecting a corticosteroid into the ischial bursa has been shown to be beneficial to some patients with chronic hamstring tendinopathy. 5 Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med 2008;36:1110-5. The ischial bursa is a small, fluid-filled structure that acts as a buffer between the overlying gluteal muscles and hamstring tendons at the sit bone (ischial tuberosity). A doctor uses ultrasound to help guide the injections of anesthetic and corticosteroid solutions into the bursa.
Cortisone injections should not be made directly into a tendon, because cortisone can damage tendon tissue over time; however, there is no reliable literature documenting this potential negative outcome with peritendinous (around the tendon) injections. 1 Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med 2009;37:727-34. , 4 Zissen M, Wallace G, Stevens K, Fredericson M, Beaulieu C. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol 2010;195:993-8. Qualified practitioners can now use ultrasound to guide the needle into the ischial bursa and avoid inadvertent placement of steroid into the tendon or the sciatic nerve. Ultrasound has greatly improved the safety and accuracy of steroid injections. 6 Hall MM, Mautner K. Evolution of musculoskeletal and non-musculoskeletal sports ultrasound. Br J Sports Med. 2015 Feb;49(3):139-40. doi: 10.1136/bjsports-2014-094192.
Ultrasound-Guided Needle Tenotomy
This in-office procedure is done using ultrasound guidance and may be an option for patients with refractory symptoms. The physician will first numb (anesthetize) the area and the needle track and tendon using local numbing medicine. Following this, the physician, using ultrasound guidance, introduces a slightly larger needle into the tendon and manipulates it in a back-and-forth motion to create bleeding and tissue damage, bringing blood and platelets to the area, with a goal of promoting new growth factors and healing. 7 Finnoff J, Fowler S, Lai J, et al. Treatment of chronic tendinopathy with ultrasound-guided needle tenotomy and platelet-rich plasma injection. PM R 2011;3:900-11. , 8 Chiavaras M, Jacobson J. Ultrasound-guided tendon fenestration. Semin Musculoskelt Radiol 2013;17:85-90. , 9 Housner J, Jacobson J, Misko R. Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med 2009;28:1187-92. , 10 McShane J, Nazarian L, Harwood M. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow. J Ultrasound Med 2006;25:1281-9. , 11 McShane J, Shah V, Nazarian L. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med 2008;27:1137-44. , 12 Testa V, Capasso G, Benazzo F, Maffulli N. Management of Achilles tendinopathy by ultrasound-guided percutaneous tenotomy. Med Sci Sports Exerc 2002;34:573-80. The use of ultrasound-guided needle tenotomy for chronic tendinopathies has been reported with good success and represents another possible treatment option for patients with recalcitrant tendinopathies. 4 Zissen M, Wallace G, Stevens K, Fredericson M, Beaulieu C. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol 2010;195:993-8. , 7 Finnoff J, Fowler S, Lai J, et al. Treatment of chronic tendinopathy with ultrasound-guided needle tenotomy and platelet-rich plasma injection. PM R 2011;3:900-11. , 8 Chiavaras M, Jacobson J. Ultrasound-guided tendon fenestration. Semin Musculoskelt Radiol 2013;17:85-90. , 9 Housner J, Jacobson J, Misko R. Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med 2009;28:1187-92. , 10 McShane J, Nazarian L, Harwood M. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow. J Ultrasound Med 2006;25:1281-9. , 11 McShane J, Shah V, Nazarian L. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med 2008;27:1137-44. , 12 Testa V, Capasso G, Benazzo F, Maffulli N. Management of Achilles tendinopathy by ultrasound-guided percutaneous tenotomy. Med Sci Sports Exerc 2002;34:573-80.
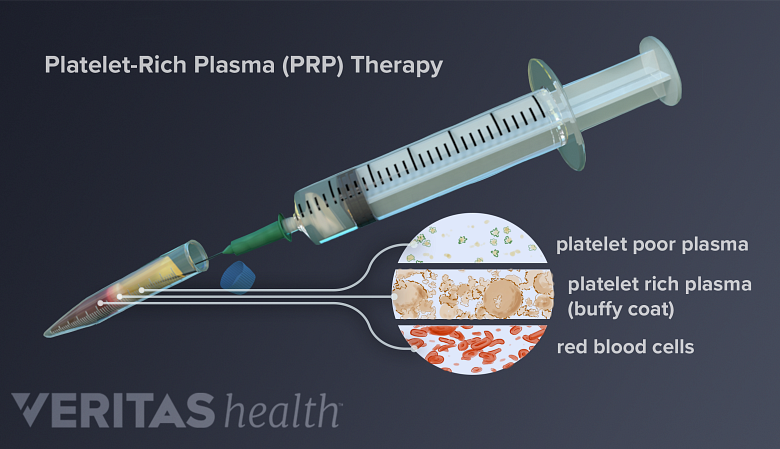
Platelet-Rich Plasma (PRP) Injections
PRP uses the patient's blood to repair damaged tissues like cartilage, tendons, ligaments, and muscles.
Ultrasound-guided tendinous injection of platelet-rich plasma (PRP), with or without needle tenotomy, has emerged as a promising treatment of tendinopathies. 4 Zissen M, Wallace G, Stevens K, Fredericson M, Beaulieu C. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol 2010;195:993-8. , 7 Finnoff J, Fowler S, Lai J, et al. Treatment of chronic tendinopathy with ultrasound-guided needle tenotomy and platelet-rich plasma injection. PM R 2011;3:900-11. , 13 Rettig A, Meyers S, Bhadra A. Platelet-Rich Plasma in Addittion to Rehabilitation for Acute Hamstring Injuries in NFL Players: Clinical Effects and Time to Return to Play. OJS 2013;1:1-5. , 14 de Jonge S, de Vos R, Weir A, et al. One-year follow-up of platelet-rich plasma treatment in chronic Achilles tendinopathy: a double-blind randomized placebo-controlled trial. Am J Sports Med 2011;39:1623-9. , 15 Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari P, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. int Orthop 2010;34:909-15. , 16 Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006;34:1774-80. , 17 Mishra A, Woodall J, Vieira A. Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med 2009;28:113-25. PRP most simply defined is a volume of platelet count that is above a patients normal blood levels of platelets. 18 Marx R. Platelet-rich plasma: evidence to support its use. J Oral Maxxilo Fac Surg 2004;62:489-96. , 1 Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med 2009;37:727-34. This is an office-based procedure that requires the patient’s own blood, which is drawn and put into a centrifuge to separate it into layers. The concentrated platelet layer is then put into a syringe and injected into the damaged area under sonographic guidance. Platelets are the body’s “healing cells” and when injected release a multitude of “growth factors” that have regenerative and healing properties. 17 Mishra A, Woodall J, Vieira A. Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med 2009;28:113-25. , 19 Pourcho AM, Smith J, Wisniewski SJ, Sellon JL. Intraarticular platelet-rich plasma injection in the treatment of knee osteoarthritis: review and recommendations. Am J Phys Med Rehabil. 2014 Nov;93(11 Suppl 3):S108-21. , 20 Creaney L, Hamilton B. Growth factor delivery methods in the management of sports injuries: the state of play. Br J Sports Med 2008;42:314-20. , 21 Foster T, Puskas B, Mandelbaum B, Gerhardt M, Rodeo S. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med 2009;37:2259-72. , 22 Anitua E, Sánchez M, Nurden A, Zalduendo M, de la Fuente M., Azofra J, Andía I. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford) 2007;46:1769-72. , 23 Boswell SC, BJ., Sundman EK, V. , Fortier L. Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy 2012;28:429-39. In general, it is believed that PRP, by releasing of growth factors locally into a damaged tendon, will induce tissue healing and regeneration. 19 Pourcho AM, Smith J, Wisniewski SJ, Sellon JL. Intraarticular platelet-rich plasma injection in the treatment of knee osteoarthritis: review and recommendations. Am J Phys Med Rehabil. 2014 Nov;93(11 Suppl 3):S108-21. Patients are usually told to avoid non-steroidal anti-inflammatories, such as aspirin, ibuprofen, naproxen, and celecoxib (Celebrex) for 7 to 10 days prior to the injection, as these medications bind platelets and temporarily inactivate them. This would essentially result in pre-deactivation of the PRP that was being used in the treatment.
See PRP Therapy for Chronic Tendon Injuries
PRP has been shown to be beneficial in improving function and reducing pain in patients with tendinopathies and has consistent level 1 data for treatment of “tennis elbow” (lateral epicondylitis). 14 de Jonge S, de Vos R, Weir A, et al. One-year follow-up of platelet-rich plasma treatment in chronic Achilles tendinopathy: a double-blind randomized placebo-controlled trial. Am J Sports Med 2011;39:1623-9. , 15 Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari P, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. int Orthop 2010;34:909-15. , 16 Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006;34:1774-80. , 24 Mautner K, Colberg R, Malanga G, et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. PM R 013;5:169-75. , 25 Thanasas C, Papadimitriou G, Charalambidis CP, I., Papanikolaou A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med 2011;39:2130-40. Recently, it has also been used effectively with good results in patients with persistent high (proximal) hamstring tendinopathy. 4 Zissen M, Wallace G, Stevens K, Fredericson M, Beaulieu C. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol 2010;195:993-8. , 13 Rettig A, Meyers S, Bhadra A. Platelet-Rich Plasma in Addittion to Rehabilitation for Acute Hamstring Injuries in NFL Players: Clinical Effects and Time to Return to Play. OJS 2013;1:1-5. , 26 Wetzel R, Patel R, Terry M. Platelet-rich plasma as an effective treatment for proximal hamstring injuries. Orthopedics 2013;36:e64-70. The patient should be aware that PRP can be extremely painful immediately following the injection and for the first two weeks. This is believed to occur secondary to the large amount of inflammatory cells being injected into a small area. The patient should also be aware that PRP can take some time to work and typically has the most benefit 6 to 12 weeks after treatment. 14 de Jonge S, de Vos R, Weir A, et al. One-year follow-up of platelet-rich plasma treatment in chronic Achilles tendinopathy: a double-blind randomized placebo-controlled trial. Am J Sports Med 2011;39:1623-9. , 15 Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari P, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. int Orthop 2010;34:909-15. , 16 Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006;34:1774-80. , 19 Pourcho AM, Smith J, Wisniewski SJ, Sellon JL. Intraarticular platelet-rich plasma injection in the treatment of knee osteoarthritis: review and recommendations. Am J Phys Med Rehabil. 2014 Nov;93(11 Suppl 3):S108-21. , 24 Mautner K, Colberg R, Malanga G, et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. PM R 013;5:169-75. While it's not considered standard practice, PRP represents a viable emerging minimally invasive treatment option for patients who have not found success with non-invasive (conservative) management. Further investigations into PRP's long term benefit and effects on proximal hamstring tendinopathy are needed and ongoing.
Ultrasound-Guided Percutaneous Needle Tenotomy (Tenex Procedure)
In 2011, the FDA approved needle ultrasonic tenotomy, sometimes called the fenestration and removal of scar tissue (FAST) procedure, for the treatment of tendinopathies. 27 Koh J, Mohan PH, TS., Lee B, Chia S, Yang Z, Morrey B. Fasciotomy and surgical tenotomy for recalcitrant lateral elbow tendinopathy: early clinical experience with a novel device for minimally invasive percutaneous microresection. Am J Sports Med 2013;41:636-44. , 28 Barnes D, Beckley J, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2014(14):S1058-2746 , 29 Pourcho AM, Hall MM. Percutaneous Ultrasonic Fasciotomy for Refractory Plantar Fasciopathy After Failure of a Partial Endoscopic Release Procedure. PM R. 2015 Apr 7. pii: S1934-1482(15)00182-3 This technology is similar to the technology used to remove cataracts from the eyes. 28 Barnes D, Beckley J, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2014(14):S1058-2746
This procedure is performed in the office or outpatient surgery center. The physician starts by numbing the skin and procedure site. Following this, the physician makes a small puncture in the skin with a scalpel, and the device is inserted into a diseased tendon under sonographic guidance. The device itself is then turned on and has a tip that vibrates at a rapid rate, emulsifying tissue in front of it and irrigating it through an outflow suction. 27 Koh J, Mohan PH, TS., Lee B, Chia S, Yang Z, Morrey B. Fasciotomy and surgical tenotomy for recalcitrant lateral elbow tendinopathy: early clinical experience with a novel device for minimally invasive percutaneous microresection. Am J Sports Med 2013;41:636-44. , 28 Barnes D, Beckley J, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2014(14):S1058-2746
Theoretically, by removing the diseased tissue—similar to a decubitus ulcer treatment—the body can then lay down new tissue. There is emerging evidence that this procedure may be superior to the traditional surgical management with a large incision. 29 Pourcho AM, Hall MM. Percutaneous Ultrasonic Fasciotomy for Refractory Plantar Fasciopathy After Failure of a Partial Endoscopic Release Procedure. PM R. 2015 Apr 7. pii: S1934-1482(15)00182-3 Further research on long-term outcomes is ongoing.
- 1 Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med 2009;37:727-34.
- 2 Puranen J, Orava S. The hamstring syndrome--a new gluteal sciatica. Ann Chir Gynaecol 1991;80:212-4.
- 3 Fredericson M, Moore W, Guillet M, Beaulieu C. High Hamstring Tendinopathy in Runners: Meeting the Challenges of Diagnosis, Treatment, and Rehabiliation. Phys Sports Med 2005;33:32-43.
- 4 Zissen M, Wallace G, Stevens K, Fredericson M, Beaulieu C. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol 2010;195:993-8.
- 5 Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med 2008;36:1110-5.
- 6 Hall MM, Mautner K. Evolution of musculoskeletal and non-musculoskeletal sports ultrasound. Br J Sports Med. 2015 Feb;49(3):139-40. doi: 10.1136/bjsports-2014-094192.
- 7 Finnoff J, Fowler S, Lai J, et al. Treatment of chronic tendinopathy with ultrasound-guided needle tenotomy and platelet-rich plasma injection. PM R 2011;3:900-11.
- 8 Chiavaras M, Jacobson J. Ultrasound-guided tendon fenestration. Semin Musculoskelt Radiol 2013;17:85-90.
- 9 Housner J, Jacobson J, Misko R. Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med 2009;28:1187-92.
- 10 McShane J, Nazarian L, Harwood M. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow. J Ultrasound Med 2006;25:1281-9.
- 11 McShane J, Shah V, Nazarian L. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med 2008;27:1137-44.
- 12 Testa V, Capasso G, Benazzo F, Maffulli N. Management of Achilles tendinopathy by ultrasound-guided percutaneous tenotomy. Med Sci Sports Exerc 2002;34:573-80.
- 13 Rettig A, Meyers S, Bhadra A. Platelet-Rich Plasma in Addittion to Rehabilitation for Acute Hamstring Injuries in NFL Players: Clinical Effects and Time to Return to Play. OJS 2013;1:1-5.
- 14 de Jonge S, de Vos R, Weir A, et al. One-year follow-up of platelet-rich plasma treatment in chronic Achilles tendinopathy: a double-blind randomized placebo-controlled trial. Am J Sports Med 2011;39:1623-9.
- 15 Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari P, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. int Orthop 2010;34:909-15.
- 16 Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006;34:1774-80.
- 17 Mishra A, Woodall J, Vieira A. Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med 2009;28:113-25.
- 18 Marx R. Platelet-rich plasma: evidence to support its use. J Oral Maxxilo Fac Surg 2004;62:489-96.
- 19 Pourcho AM, Smith J, Wisniewski SJ, Sellon JL. Intraarticular platelet-rich plasma injection in the treatment of knee osteoarthritis: review and recommendations. Am J Phys Med Rehabil. 2014 Nov;93(11 Suppl 3):S108-21.
- 20 Creaney L, Hamilton B. Growth factor delivery methods in the management of sports injuries: the state of play. Br J Sports Med 2008;42:314-20.
- 21 Foster T, Puskas B, Mandelbaum B, Gerhardt M, Rodeo S. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med 2009;37:2259-72.
- 22 Anitua E, Sánchez M, Nurden A, Zalduendo M, de la Fuente M., Azofra J, Andía I. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford) 2007;46:1769-72.
- 23 Boswell SC, BJ., Sundman EK, V. , Fortier L. Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy 2012;28:429-39.
- 24 Mautner K, Colberg R, Malanga G, et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. PM R 013;5:169-75.
- 25 Thanasas C, Papadimitriou G, Charalambidis CP, I., Papanikolaou A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med 2011;39:2130-40.
- 26 Wetzel R, Patel R, Terry M. Platelet-rich plasma as an effective treatment for proximal hamstring injuries. Orthopedics 2013;36:e64-70.
- 27 Koh J, Mohan PH, TS., Lee B, Chia S, Yang Z, Morrey B. Fasciotomy and surgical tenotomy for recalcitrant lateral elbow tendinopathy: early clinical experience with a novel device for minimally invasive percutaneous microresection. Am J Sports Med 2013;41:636-44.
- 28 Barnes D, Beckley J, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2014(14):S1058-2746
- 29 Pourcho AM, Hall MM. Percutaneous Ultrasonic Fasciotomy for Refractory Plantar Fasciopathy After Failure of a Partial Endoscopic Release Procedure. PM R. 2015 Apr 7. pii: S1934-1482(15)00182-3