Frozen shoulder (adhesive capsulitis) often affects adults between the ages of 40 and 60,1Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016. but this condition can occur at any age. In addition to age, risk factors include:
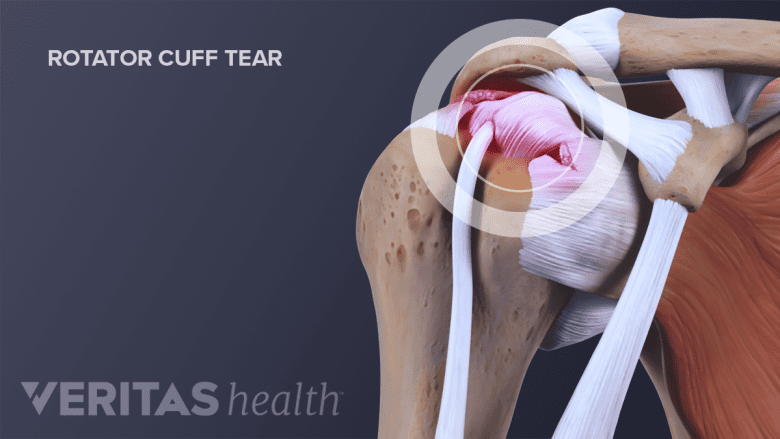
Frozen shoulder may coexist with other shoulder issues, such as a rotator cuff tear.
In This Article:
- What to Know About Frozen Shoulder
- Frozen Shoulder Symptoms
- Frozen Shoulder Causes and Risk Factors
- Diagnosing Frozen Shoulder
- Treating Frozen Shoulder
Gender. Women are more likely to develop frozen shoulder. Experts suspect this is due to changes in hormone levels, such as menopause.
Diabetes. People with diabetes have a higher rate of frozen shoulder—10% to 20%1Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016. —compared to the general population, which is about 2%.1Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016. The exact reason for this increase is not known, but some experts theorize that glucose molecules (sugar) attach to the collagen proteins naturally found in the shoulder joint capsule, causing stiffness. People with diabetes are also more likely to develop this condition in both shoulders.
Other diseases and conditions. In addition to diabetes, other health issues increase the risk of developing frozen shoulder, including:
- Thyroid problems (hypothyroidism and hyperthyroidism)
- Depression
- Cardiovascular disease
- Lung disease
- Breast cancer
- Open heart surgery
- Polymyalgia rheumatica (an inflammatory condition causing stiffness and muscle discomfort)
- Parkinson’s disease
Shoulder stiffness may be one of the first indications of Parkinson’s.2Ford B. Pain in Parkinson's Disease. Center for Parkinson’s Disease & Other Movement Disorders Columbia University Medical Center. Winter 2004-2005. http://www.pdf.org/en/winter04_05_Pain_in_Parkinsons_Disease Accessed May 25, 2016. There have also been incidences of frozen shoulder in people who have had either lung or breast cancers.
Periods of inactivity. Long periods of inactivity—from an injury, surgery, stroke, or illness—can lead to frozen shoulder. People may be susceptible to inflammation or develop stiff tissue during these times. Completing physical therapy exercises following shoulder surgery can help prevent this condition.
Other shoulder issues. Frozen shoulder can occur alongside other shoulder problems, including:3Frozen shoulder causes. National Health Services website.http://www.nhs.uk/Conditions/Frozen-shoulder/Pages/Causes.aspx. Last reviewed March 17, 2016. Accessed August 12, 2016.
- Calcific tendonitis, or calcium deposits in the rotator cuff.
- Rotator cuff tear, or injury to the large tendon in the shoulder comprised of four muscles.
Stiffness may also occur in patients who have undergone shoulder surgery such as rotator cuff or labral repairs, or in patients with shoulder fractures, arthritis, and shoulder instability.
Previous case of frozen shoulder. Frozen shoulder typically resolves with time. However, once frozen shoulder has been resolved, the opposite shoulder becomes affected in 6% to 17% of patients within 5 years.4Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ : British Medical Journal. 2005;331(7530):1453-1456. Found in Rizk TE, Pinals RS. Frozen shoulder. Seminars Arthritis Rheumatism 1982;11: 440-52.
There are conflicting opinions about whether frozen shoulder is more likely to develop in the dominant or non-dominant arm. Some experts believe frozen shoulder develops in the non-dominant arm. Others suggest there is no link arm dominance and frozen shoulder.1Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016.
When frozen shoulder occurs without an identifiable cause, it is called primary adhesive capsulitis. When frozen shoulder is triggered by an event or disease, it is called secondary adhesive capsulitis.
- 1 Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016.
- 2 Ford B. Pain in Parkinson's Disease. Center for Parkinson’s Disease & Other Movement Disorders Columbia University Medical Center. Winter 2004-2005. http://www.pdf.org/en/winter04_05_Pain_in_Parkinsons_Disease Accessed May 25, 2016.
- 3 Frozen shoulder causes. National Health Services website.http://www.nhs.uk/Conditions/Frozen-shoulder/Pages/Causes.aspx. Last reviewed March 17, 2016. Accessed August 12, 2016.
- 4 Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ : British Medical Journal. 2005;331(7530):1453-1456. Found in Rizk TE, Pinals RS. Frozen shoulder. Seminars Arthritis Rheumatism 1982;11: 440-52.

