People who have frozen shoulder often experience shoulder pain, stiffness, and decreased range of motion. Everyday activities—such as getting dressed or reaching for something in a cupboard—can be challenging.
About 2% of the population is affected by frozen shoulder.1Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016. It often impacts adults aged 40 to 60,1Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016. and is more common in women and people with certain medical conditions, such as diabetes.
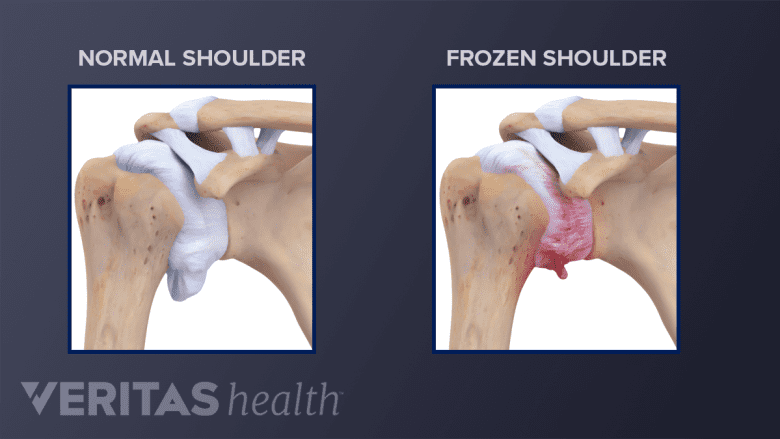
Symptoms are felt when the shoulder joint capsule, composed of ligaments surrounding the shoulder joint, becomes inflamed and thickens, restricting movement. Early on, frozen shoulder symptoms (pain and limited motion) are similar to symptoms of other shoulder conditions—including labral tears and rotator cuff tears—making diagnosis a process of elimination.2Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1(3-4):180-9.
See Soft Tissues of the Shoulder
Frozen shoulder is also referred to by its medical name, adhesive capsulitis.
In This Article:
- What to Know About Frozen Shoulder
- Frozen Shoulder Symptoms
- Frozen Shoulder Causes and Risk Factors
- Diagnosing Frozen Shoulder
- Treating Frozen Shoulder
How Does Frozen Shoulder (Adhesive Capsulitis) Occur?
Frozen shoulder occurs when:
- The inflammation of the joint capsule causes the shoulder ligaments to swell and thicken,3Adhesions in the Shoulder. PubMed Health website. Accessed May 22, 2016. resulting in scar tissue, sometimes called adhesions. This leaves less space for the ball of the shoulder joint—the humeral head—to rotate in its socket, causing shoulder stiffness and pain.
- There is a decrease in the shoulder joint’s lubricating synovial fluid which reduces joint friction and helps facilitate joint movement.
These changes occur over time and do not necessarily occur in a specific order. Eventually, the shoulder’s movement becomes more limited.
3 Phases of Frozen Shoulder
Frozen shoulder has three different phases. Each phase can last several weeks to months. The three phases are:
- Freezing, with pain increasing over time
- Frozen, when stiffness is the primary symptom and shoulder pain may decrease
- Thawing, when shoulder strength and motion completely or partially return to normal
Many people with frozen shoulder do not need surgery and can reduce shoulder pain and regain movement with nonsurgical treatments, such as injections and physical therapy.
Primary vs. Secondary Causes
Doctors sometimes describe frozen shoulder as either primary or secondary adhesive capsulitis:4Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010;5(4):266-73.
- Primary adhesive capsulitis (idiopathic) is an inflammatory reaction, which may possibly be genetic, occurring without an identifiable cause.
- Secondary adhesive capsulitis is when the shoulder joint becomes inflamed for an identifiable reason, such as a surgery, disease, or an accident.
No matter what the cause, treatment for frozen shoulder is the same. However, if the suspected underlying cause is treatable or preventable, such as diabetes, patients are encouraged to seek additional medical care.
- 1 Frozen Shoulder. American Academy of Orthopaedic Surgeons. http://orthoinfo.aaos.org/topic.cfm?topic=a00071. Last reviewed January 2011. Accessed May 19, 2016.
- 2 Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1(3-4):180-9.
- 3 Adhesions in the Shoulder. PubMed Health website. Accessed May 22, 2016.
- 4 Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010;5(4):266-73.

